When Helpful Becomes Harmful
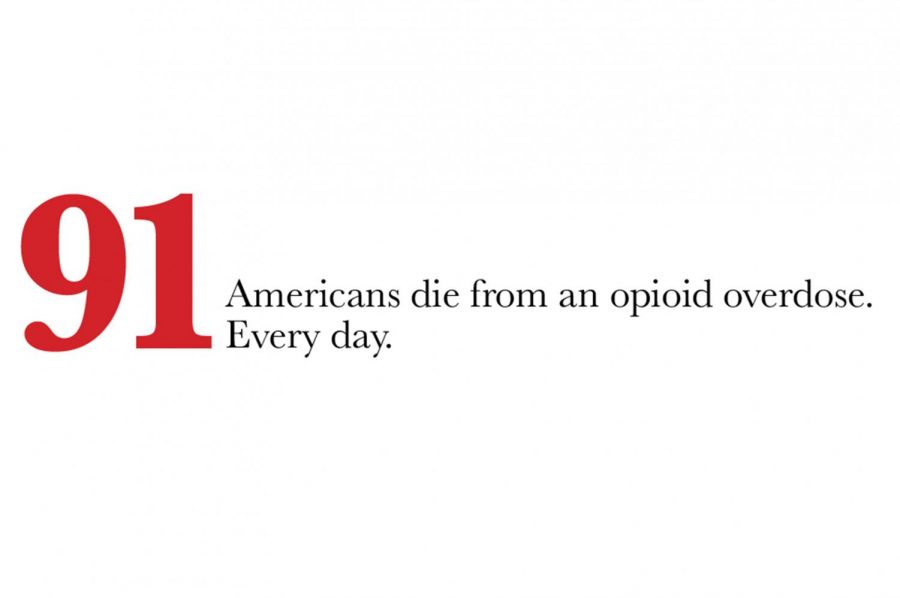
Currently, the number one cause for break-ins in the United States is for the theft of prescription drugs. These numbers might sound crazy, but Dr. Jennifer Waljee has stopped being shocked by information like this.
Dr. Jennifer Waljee, M.D., Associate Professor of Plastic Surgery at the University of Michigan, has recently become interested in opioid use, specifically as it affects her hand surgery patients. “We know that if patients are either actively on opioids, or they’ve been exposed to opioids in the year prior to surgery, they tend to not do as well after surgery,” Waljee said. “They have more complications; they’re less likely to go home; they’re more likely to be discharged to rehab facilities or nursing facilities; they overall cost the system more money; they tend to stay longer.”
There are no proven answers as to why these things happen. Hypotheses include the idea that opioids are immunosuppressants , which hinder the body’s response to physiologic stress, like surgery. There is also the fact that if one is taking opioids, even stronger doses than usual will be necessary to manage pain; this can lead to other problems that can slow down recovery after a surgery.
Her initial curiosity stemmed from the following question: “How do we know how much we’re supposed to prescribe our patients?”
With all the guidelines in medicine, it may come as a surprise that there are few guidelines for this. During the time of Waljee’s training, a new concept was evolving: along with body temperature, heart rate, respiratory rate, and blood pressure, pain should be considered as the fifth vital sign. Patients, families, and even healthcare providers often believe that the healthcare experience should be pain-free. Early marketing around prescription opioids said they were not addictive, and if taken for acute pain purposes one could not become dependant on them.
“It was thought that we would have license to prescribe them pretty liberally after surgery,” Waljee said. “If you prescribe too many, it would be fine because if patients didn’t have acute pain they wouldn’t take them and it wouldn’t be a big deal. They were thought to be pretty safe. That turned out not to be true at all.”
Waljee has been doing this research for the last two years with Dr. Mike Englesbe, a fellow surgeon, and Dr. Chad Brummett, Director of the Division of Pain Research. They are focusing on two main issues.
The first concern returns to Waljee’s original question: “How do we know how much we’re supposed to prescribe our patients?” Waljee admits that although most people have reported that they take three to five pills after a surgery, doctors still prescribe 30 or 40, on average. Waljee wants to find out how many pills people should ideally be prescribed; she wants to educate doctors on how to prescribe in a way that is more aligned with what the data shows patients are actually taking, and even see if patients can manage their pain without opioids at all.
The second problem relates to the disposal of the excess opioids. Extra pills are sometimes kept in a medicine cabinet at home for months, or even years. “People hang onto them for a variety of reasons, either because they just forget about them or they think that they might need them in the future if they have a toothache, or a headache, or whatever; they don’t want to have to go back and ask for another prescription from a provider,” Waljee said.
One reason for this tends to be the high out-of-pocket cost of prescription opioids. Another may be people just forgetting that they still have them; Waljee herself said she had a few leftover from one of her C-sections. “Although I would say honestly the biggest reason is just lack of awareness of how dangerous they can be,” Waljee said.
Studies have shown that the majority of people who use heroin were initially exposed to prescription opioids, either their own or those prescribed to a friend or family member. “It’s not necessarily they wake up and start buying them off the street from a drug dealer,” Waljee said.
Disposing of the excess medications is not as simple as throwing them in the garbage or down the drain. Some people have proposed flushing them down the toilet, but that contaminates the water supply; many communities offer a program where people can drop them at the sheriff’s office or other law enforcement agency, but that is not always convenient; they can sometimes be returned to pharmacies or hospitals/clinics, but not all places take them back. So the newest question Waljee and her colleagues are looking into is what should be done with these extra pills?
Since researching this topic, Waljee finds she approaches her patients differently. She continues to prescribe opioids, but in smaller amounts. The main change she has made is having a conversation with her patients about their pain management and expectations. She discusses what they think they might need, based on their prior experiences, how many pills they have needed in the past if they have had a previous surgery, and what their experience was like with opioids. To her surprise, many people respond with things like, “I don’t need anything, I have some in my medicine cabinet from my last five procedures that I never took.” With these patients, she either prescribes very few pills — or even none.
As is apparent from the increasing amount of media attention, as well as the stance our current administration has taken, this is a very complicated problem. Physicians walk a thin line between appropriately treating pain and contributing to the worsening opioid epidemic. As Waljee notes, there are many ways you can approach opioid research: from the perspective of chronic pain, from the perspective of addiction, or from the perspective of overprescription, to name a few. “I don’t want to portray the message that opioids aren’t good for pain when used appropriately under the control of a physician, but I think it’s important to know that they are not without risks, and it’s important to dispose of them safely.”

Her life outside of the journalism lab consists of one thing: gymnastics. It takes up all of Abbie’s “free time,” but she wouldn’t be who she is today without having spent almost 13 years in the sport. Abbie also loves listening to music — believing that there is at least one song for whatever mood someone is in — and spends much of her money on going to concerts, her happy place. She simultaneously wants May (aka graduation) to come quickly, but also take its time; clearly, she’s terrible at making decisions, so it’s a good thing she has three other editors to help her through this crazy process!